
STAYING ON TRACK
Intensive diabetes management and continuous glucose monitoring

Technology has evolved a lot for people with type 1 diabetes, but is it right for you?
If you have type 1 diabetes or are the care partner of someone who does, you may have heard about continuous glucose monitoring (CGM) and intensive diabetes management. But it’s not always easy to know whether—or when—it’s the right time to use these diabetes treatment tools.
Here’s some information that may help you make the right decision for yourself or the person you care for along with your diabetes care teamDiabetes care teamYour diabetes care team may include a primary care doctor, a diabetes and hormone doctor (endocrinologist), a registered nurse, a diabetes educator, a dietitian, a heart doctor (cardiologist), a foot doctor (podiatrist), an eye doctor (ophthalmologist/optometrist), a kidney doctor (nephrologist), a dentist, a pharmacist, and a mental health professional. .

In the 1970s, finger-stick blood glucoseBlood glucoseThe main sugar found in the blood, and the body’s main source of energy. monitoring was developed. Since then, it has become widely used for checking blood glucose.
More recently, the Food and Drug Administration (FDA) has approved real-time CGM. A CGM is a small sensor inserted under the skin that measures the fluid between cells called interstitial fluid. This measure is closely related to blood glucose, so it can be used to measure blood glucose levels.
The benefits of CGM include:
- CGM gives you an almost continuous readout of blood glucose levels, displaying them every 1 to 5 minutes. So, you can see whether blood glucose is rising or falling. You can’t tell this with a finger-stick reading since it is only a snapshot of your blood glucose level
- Knowing which way blood glucose is going can be helpful. For instance, when trying to figure out if you (or the person you care for) need a snack before bedtime. If your blood glucose is where it should be, but is falling, then maybe a snack is a good idea to keep it from going too low. But, if it’s going up, a snack is probably not needed or helpful
- CGM has a built-in alarm warning that signals when blood glucose levels get too high or low. This helps people with diabetes find their way out of the danger zone. It may be really useful for those with low blood glucose unawareness. If you are thinking about trying tight controlTight controlIntensive insulin therapy is a treatment approach designed to keep your blood glucose levels closer to the levels of someone who doesn’t have diabetes. This treatment requires close monitoring of blood glucose levels and multiple doses of insulin., but are afraid of hypoglycemia, CGM may be especially helpful
- CGM provides much more information than finger-stick readings alone. The detailed information CGM gives you about how blood glucose changes helps you figure out patterns, so you can fine-tune food choices and insulin InsulinA hormone made by the beta cells in the pancreas that helps glucose move from the blood into the cells. Insulin is also an injectable medicine that is used to treat diabetes by controlling the level of glucose in the blood.doses
- You'll know if you're meeting your "time-in-range" target. The ADA recommends that people using CGM stay within their recommended target range 70% of the time. So for most nonpregnant adults, that means 16.8 hours a day between 70 mg/dL and 180 mg/dL to keep A1C below 7%.
Here are some other things to remember about CGM:

CGM does not replace finger-stick measurements. Finger-stick readings are more accurate than CGM readings and are needed to calibrate CGM measurements. And it is still necessary to confirm CGM readings with a finger stick before taking a bolusBolusBolus insulin (prandial or mealtime insulin) is insulin taken to cover an expected rise in blood glucose resulting from a meal or snack. It can also be taken when blood glucose is high. of fast‑acting insulin

CGM can be a constant reminder of diabetes. Instead of thinking about your diabetes mainly when checking blood glucose and taking insulin, new blood glucose measurements will be showing up every few minutes. While some people may find that reassuring, it can be too much information for others

CGM can be expensive, especially when it is not covered by insurance. Be sure to consult with your diabetes care team before making any changes to ensure that this is the right method for you or the person you care for
The person with diabetes, care partner, and diabetes care team work together to safely keep blood glucose levels as close as possible to the level of someone without diabetes. This is referred to as “intensive diabetes management.” However, this type of control is not for everyone. People who have a high risk of low blood glucose may be advised by their doctors to aim for slightly higher goals.
The blood glucose goals recommended by the ADA for many nonpregnant adults are:
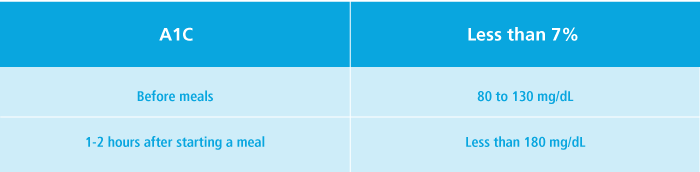
However, some doctors may set even lower blood glucose goals (such as an A1CA1CA test that gives you a picture of your average blood glucose level over the past 2 to 3 months. The results can give you an idea of how well your diabetes is being controlled. Also known as "hemoglobin A1C," the A1C test does this by measuring the amount of glucose that has attached to the hemoglobin in your red blood cells. More glucose means a higher A1C. of less than 6.5%) for people with type 1 diabetes who are likely to achieve these goals without a major risk of low blood glucose or other negative effects.
Intensive diabetes management for children and teenagers
An A1C of less than 7% is appropriate for many children and adolescents, but a child's or teen's blood glucose goals may be higher or lower depending on many factors. Consult with the diabetes care team to decide what is right for you or the person you care for.
Intensive diabetes management means being strict
Checking blood glucose levels often (perhaps more often than you’re used to) and tracking the results
Closely following eating and physical activity plans and possibly tracking food and physical activity, too
- Taking frequent doses of insulin by injection or through an insulin pump
Always do what your diabetes care team tells you
The benefits of intensive diabetes management need to be balanced against possible risks. These include low blood glucose (hypoglycemia) and potential weight gain. This type of control is not something that you or your care partner should try without the help and advice of a doctor. Talk to the diabetes care team about what makes sense for you or the person you care for.


